Nursing Clinical During COVID: Your FAQs Answered
/We are in a pandemic,
and if you are a nursing student right now, things are less than ideal.
The clinical hours spent at the bedside in a nurse’s education are vital. It’s where you practice those hands-on skills and develop comfort of patient interactions- things you simply cannot teach over zoom or on a mannequin. However since the pandemic, academic institutions and hospitals have had the unprecedented ethical consideration of valuing hands-on clinical education against the risk of COVID-19 exposure for staff and students. COVID is changing the future of nursing education and if you are currently in school, you are the guinea pigs. Awesome...
First, let me tell you that I am so sorry. I’m sorry on top of everything you need to deal with as a nursing student that this is happening. With that being said, you also are getting to learn from the true heroes of this pandemic. You are witnessing the strength of our field and nurses coming together. You are seeing healthcare workers step up, advocate for themselves and their communities. For the first time, healthcare workers are being celebrated for their undeniable dedication for the wellbeing of others and I hope you find inspiration in that.
While questions undoubtedly circle your mind, I hope as a clinical nursing instructor I can provide some insight and advice to your very well justified concerns. These opinions are my own. Always follow the guidance of your own institution or University that is taking your specific community transmission, local and state regulations into consideration.
FAQs
I’M WORRIED I FORGOT ALL OF MY CLINICAL SKILLS
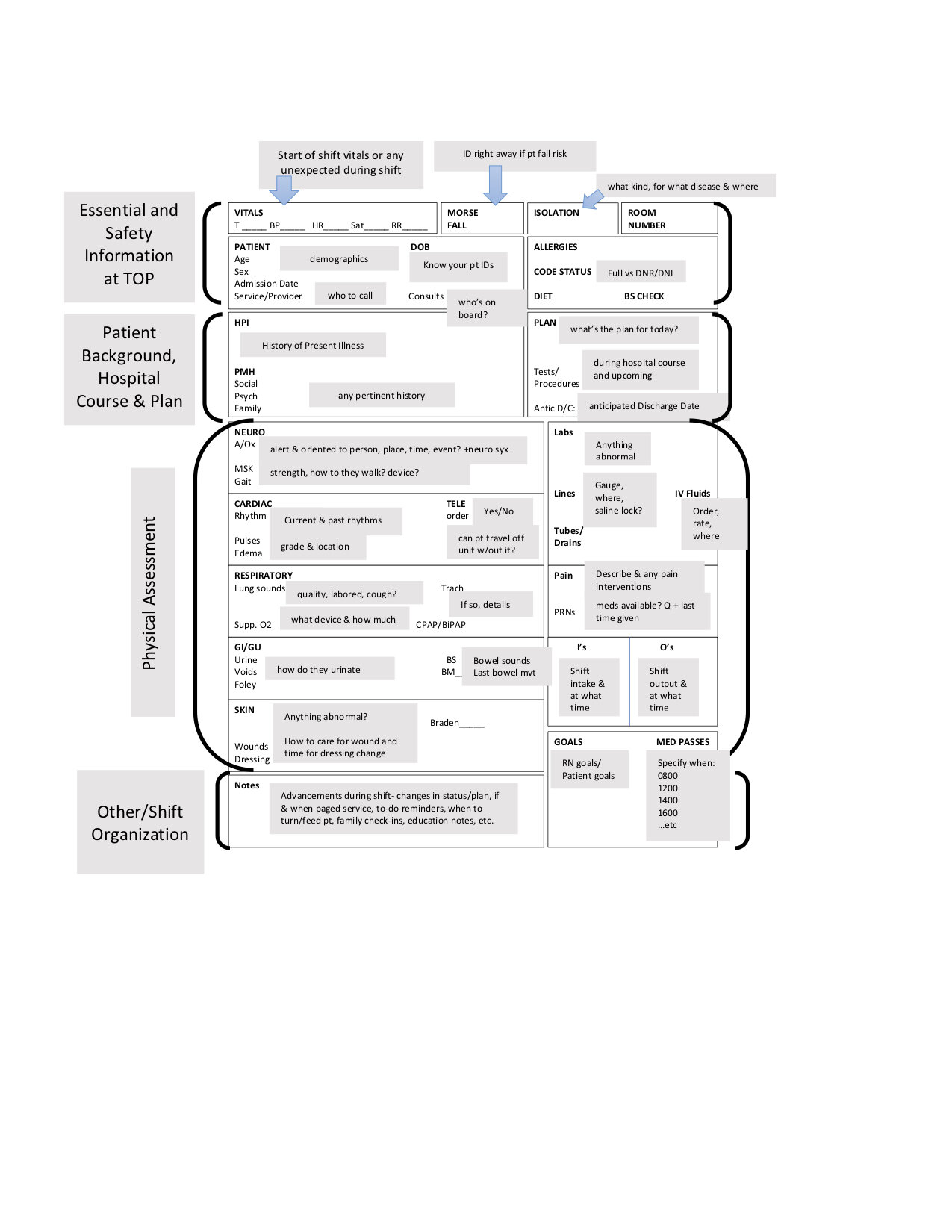
Don’t fret, you are not alone here. Your clinical instructors are well aware of the pandemic putting the last few months of clinical experiences on hold. Refresh on the most important skills before heading back: checking vitals, PPE, infection control, hand hygiene, safety and the physical assessment. Don’t put too much pressure on yourself to pick up exactly where you left off, and never hesitate to let your instructor know your concerns or ask for help.
IF WE MOVE BACK ONLINE SOON, HOW CAN I MAKE THE MOST OF MY CLINICALS NOW?
Completing complex clinical skills will come over time. As I like to tell my students, you can teach a monkey to start an IV. Right now, stick to the basics I described above, focus on your patient interactions and thinking critically about their disease processes and plans of care. Come prepared and don’t be afraid to ask questions.
For the last few months, patients have been limited with the amount of visitors allowed and probably still are! Use this as an opportunity to be a source of emotional and educational support for your patients that are most likely feeling lonely and isolated. I am sure they will love your extra company and attention.
WHAT IF ALL OF MY CLINICAL GOES VIRTUAL?
Unfortunately, we on the academic side are preparing for another COVID wave and yes, there is a strong chance we will shut back down and go to remote learning (if your institution hasn’t done so already). Take comfort knowing your faculty is keeping the health and safety of you and your loved ones a top priority. Nursing education is changing and this will most definitely be reflected in training new nurses coming out of the pandemic (hello NCLEX already adapting!). It’s your job to get through nursing school, not figure out how to get clinical hours. Save that problem for your faculty and the nursing board of licensing to figure out.
If and when virtual clinical comes, make the most of it. Come prepared, ask questions and consider a zoom study group.
I’M MISSING MY DREAM ROTATION. HOW WILL I KNOW MY SPECIALTY?
One of the most exciting parts about going through nursing school is experiencing the different specialties- peds, L&D, psych, community health, etc. Having an entire specialty rotation cut out of the mix can leave you with a lot of question and uncertainty. My personal advice: chances are if you just have a feeling peds is for you, or you just know L&D is your calling, then you are probably right.
Missing your dream NICU rotation? don’t give up!
BE PROACTIVE. Try to find outside volunteer experiences on these units now if you can or when the pandemic calms down (who knows when that will be). Reach out to those specialty clinical directors at your institution to see if they have any connections with hospitals allowing volunteers or nursing students just to shadow, even for one or two shifts. That may be enough to confirm that specialty is right for you. You can also reach out to find nurse mentors that work in that field. Pick their brains - ask what drew them to that speciality, pros/cons of that work, what a typical day is like, what recommendations they have for volunteer or work opportunities during the pandemic to get more experience.
SHOULD I GET A JOB AS A TECH/CNA TO GET HANDS ON EXPERIENCE?
This may not be a popular opinion but unless you are truly called to start working as a tech or CNA, I would proceed with major caution. Training and working as a tech/CNA is extremely demanding and the pandemic has made it even more challenging. Starting a new job, plus COVID, on top of your nursing course load is probably not a good idea right now.
However, if you are called to this work and want to help fight the good fight against COVID-19, major pat on the back to you. Do not let my opinion stop you. Nursing students that have CNA experience really have a leg-up getting comfortable with patient care and it will definitely help get you a job coming out of this potentially tricky market for new grads. If you are interested, start looking for a job now and maybe train over one of your breaks from school.
I AM ANXIOUS, STRESSED & WORRIED I MADE THE WRONG DECISION BEING A NURSE
Another thought that is extremely common for nursing students, pandemic or not. Take care of yourself by approaching your immune system holistically- prioritizing nutritious foods, hydration, exercise, sleep and self care. Whether that’s an online yoga class, journaling in the morning, downloading a meditation app like Calm or calling a loved one, find those practices now and stick to them.
However, as the months continue through the COVID-19 pandemic, increasing anxiety and depression is common for many people, especially those in healthcare with higher exposure. Know your limits, give yourself some grace and reach out to your faculty, other students and campus organizations for extra support. Most universities are offering remote counseling and support groups. See the resources at the bottom of this post for more.
I’M ABOUT TO GRADUATE AND FEEL TOTALLY UNPREPARED
Let me let you in on a little secret….Ready?
All nursing students feel completely unprepared heading into their first jobs, pandemic or not. Believe me, 99% of what you learn as a nurse will happen during the first year on the job. While clinical is a great experience to get you ready for that, the amount of learning that will happen in that first month of you working will probably be more than all of our clinicals in nursing school combined.
When applying for jobs, look for nurse residency programs that support new grads. Discuss your concerns with managers while applying because again, you are not alone. Seek mentors on your unit when you get hired and give yourself some time & patience. Your managers, preceptors and fellow nurses will know you trained during the pandemic and hopefully will give you that extra support and time that you deserve.
I’M WORRIED I WON’T BE ABLE TO FIND A JOB
That’s right, we are in a global pandemic and some nurses are having a hard time finding work. With hiring freezes and stressful work conditions, unfortunately hiring and training new grads is not at the top of many hospital’s to-do lists.
If you have a stable job already and are not itching to start your RN career, my advice is to take a break while you job search. It can take some new grads anywhere from 6-10 months before finding a job anyways (that’s why I say NETWORK, NETWORK, NETWORK when you are in school).
If you are dead set on starting a nursing job right away, try to make as many connections as possible before graduation. Reach out to old clinical instructors, instructors, faculty members about hospitals hiring new-grads. Attend virtual job fairs. If you can’t land your dream job during or after the pandemic, keep your head up. You have lots to learn in the nursing world and there are always opportunities to change units, hospitals or specialties.
I AM WORRIED ABOUT GETTING COVID ON MY CLINICAL SITE/BRINGING IT HOME TO MY FAMILY
If you are going on-site to clinical, you are not alone in your fears or stress. To get you up to speed and make sure you feel as safe as possible, check out my Tips for Staying Safe in Clinical During COVID-19. However, know that your safety is the most important and continue to advocate for yourself and your family. Express any concerns about exposure in clinical you have to faculty members and administrators.
I hope this gives you the support and comfort you need heading into clinicals. Stay safe and please do not hesitate to reach out if you have any specific questions, thoughts or ideas. Feel free to drop me a line in the comments or find me on social media, I’d love to hear from you!
XOXO,
Jac
RESOURCES
Well-Being Initiative from the American Nurses Association (ANA).
Nurses’ Guide to Mental Health Support Services
The Guide to Sleeping Better and Restoring Energy
Download the Happy App, a nurse-specific platform that gives you access to 24/7 support.
If you feel overwhelmed beyond your limits by sadness, depression, or anxiety, or if you have thought of hurting or killing yourself, call 911. You can also call or text one of these crisis hotlines for immediate response:
Crisis Text Line: Text HOME to 741741
National Suicide Prevention Lifeline: 1-800-273-TALK (8255) or Live Online Chat . If you or someone you know is suicidal or in emotional distress, contact the National Suicide Prevention Lifeline. Trained crisis workers are available to talk 24 hours a day, 7 days a week.
SAMHSA Treatment Referral Helpline: 1-877-SAMHSA7 (1-877-726-4727). Get general information on mental health and locate treatment services in your area. Speak to a live person, Monday through Friday from 8 a.m. to 8 p.m. EST.